Is Your Back Pain a Sign of Something Serious?
The situation is all too common: you bend over to pick up something simple, and suddenly, your back seizes up, leaving you barely able to move. Your first instinct might be to assume the worst—that you’ve done some irreparable damage. However, you are far from alone. Around 80% of people will experience significant back pain at some point in their lifetime. Yet, not 80% of people are walking around in severe, chronic pain, illustrating the fact that most acute back pain tends to resolve relatively quickly.
Given the intensity of the pain, consider seeing your doctor or PT or going to the ER. When you’re in such pain, it seems obvious an MRI or X-ray should be ordered immediately. However, current medical guidelines strongly advise against routine imaging unless certain red flags are present, such as bladder incontinence or leg weakness so severe that you cannot bear weight.
The Limitations of Imaging
You might think, “ I’d just feel better knowing exactly what’s going on.” While that sentiment is understandable, it does not consider the limitations of imaging techniques like MRIs. Studies have shown that MRIs frequently produce false positives, detecting abnormalities that are not clinically significant. For example, many people without any back pain at all have bulging discs or degenerative changes on MRI scans. When such incidental findings occur in a case of back pain that would have naturally improved, they can create unnecessary anxiety and lead to invasive procedures, such as surgery or injections, that may not be needed (Chou et al., 2007; Jarvik et al., 2003).
In fact, healthcare providers are often doing patients a favor by not ordering imaging right away. Clinical guidelines consistently recommend against routine imaging for uncomplicated low back pain because it does not improve outcomes and can sometimes be harmful by prompting unnecessary interventions (Chou et al., 2009; Talmage et al., 2011). In other words, most people improve without these tests, saving time and money while avoiding more invasive techniques that may not be necessary!
Are You Just Jumping Through Hoops?
As a physical therapist, I frequently hear this frustration from patients: I feel like I’m just jumping through hoops because my insurance company won’t approve an MRI until I do therapy first. While insurance policies can sometimes feel like an obstacle, in this case, they are actually aligned with best-practice care. Clinical research and guidelines from organizations such as the American College of Physicians (ACP), the American Pain Society (APS), and the National Institute for Health and Care Excellence (NICE) all emphasize that early imaging does not improve long-term outcomes for most people with acute low back pain (Chou et al., 2007; NICE, 2009).
If your symptoms persist beyond 30 to 60 days, or if you develop new concerning signs like those mentioned earlier, imaging may become necessary. Otherwise, getting an MRI or X-ray too soon may actually be detrimental to your recovery.
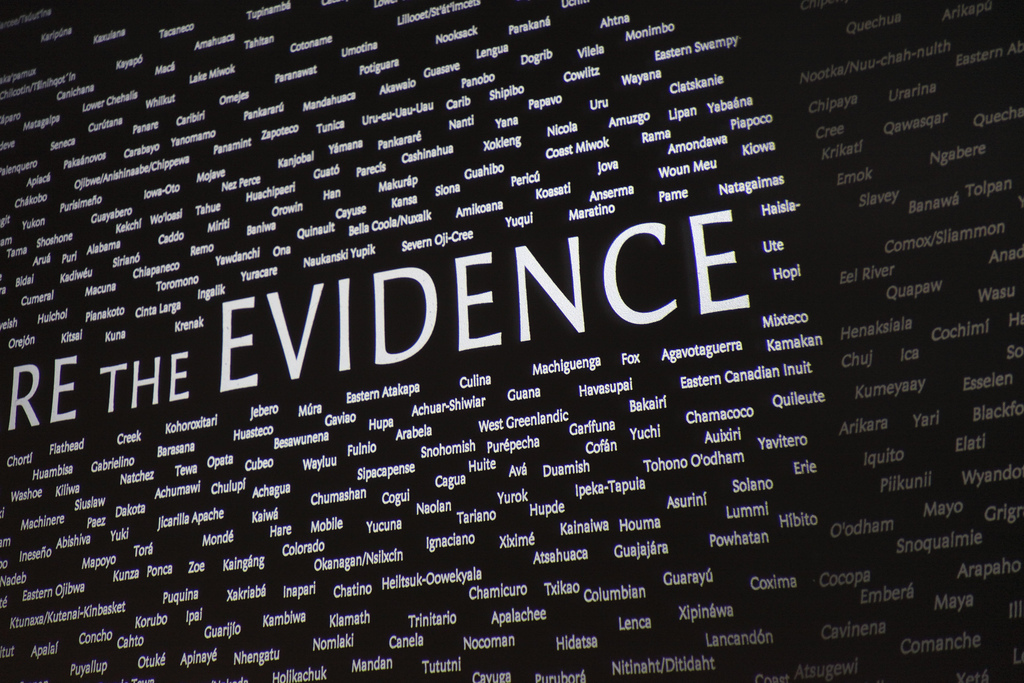
Evidence-Based Guidelines on Imaging for Low Back Pain
This recommendation is consistent across multiple professional organizations and clinical guidelines:
American College of Radiology (2011) – ACR Appropriateness Criteria® for low back pain.
American College of Physicians & American Pain Society (2007) – Joint clinical practice guideline emphasizing that imaging should only be used when serious conditions are suspected (Chou et al., 2007).
Systematic Review & Meta-Analysis (2009) – Found that routine imaging does not improve clinical outcomes for most patients with low back pain (Chou et al., 2009).
JAMA Randomized Controlled Trial (2003) – Demonstrated that rapid MRI versus radiographs for low back pain did not improve treatment outcomes (Jarvik et al., 2003).
Occupational Medicine Practice Guidelines (2011) – Reiterated that early imaging is not beneficial in most low back pain cases (Talmage et al., 2011).
NICE Low Back Pain Guideline (2009) – Advised against unnecessary imaging in the absence of red-flag symptoms.
The Bottom Line
If your doctor does not immediately order an MRI or X-ray for your back pain, it is not because they are dismissing your concerns. Instead, they are following evidence-based guidelines designed to ensure you receive the safest, most effective care. Early imaging often leads to overdiagnosis and unnecessary procedures, which can ultimately do more harm than good.
What is your best course of action? Follow your healthcare provider’s recommendations, engage in appropriate physical therapy, and allow time for natural healing. If your symptoms persist or worsen, then imaging may be needed. But in most cases, patience and conservative care are the best medicine.
Photo by Photo By: Kaboompics.com: https://www.pexels.com/photo/doctor-examines-woman-s-back-4506109/