By Andy Parsons, PT, DPT, OCS
In 2016, A cochrane systematic review compared conservative management after ACL tear to ACL reconstruction (ACLR).1 The review concluded that ACLR did not show superior outcomes compared to conservative management up to five years after the initial injury.1,2 Prior practice standards indicated ACLR based on age and activity level; younger patients generally had ACLR, and older individuals might forego the procedure. This could be the beginning of a paradigm shift for management of ACL lesions because some active individuals seem to perform well with conservative care alone.
Copers and Non-copers
The new paradigm is based on a subset of individuals with an ACL deficient knee that “cope” without the inherent ligamentous stability of the ACL. The “coper” group likely gets their knee stability “dynamically” from the muscle groups surrounding the knee as neuromuscular activation patterns change to provide stability to the ACL deficient knee. Non-copers do not function well without the passive restraints of the ACL, and surgery would be indicated in this group.
Once a Coper Always a Coper?
The literature is still trying to answer many questions regarding the feasibility of conservative management in this population. Even though we might be able to classify a patient as a coper or non-coper, there is no guarantee that the individual will remain in one discrete group.
In the primary study of conservatively managed ACL ruptures, 39% opted for ACLR by two years and 51% opted for surgery by five years due to knee instability (these groups were randomized and diagnostically selected for surgical or conservative care). However, in another study, 70% of subjects initially classified as non-copers were functioning well without ACLR at one year following non-operative treatment.3
A Shift Towards a New Paradigm?
Proposed criteria for classifying patients as a coper:3
Hop test of >80% for timed 6m hop test comparing contralaterally
KOS-ADLS score >80%
Global rating of function >80
No more than one episode of knee giving way since injury
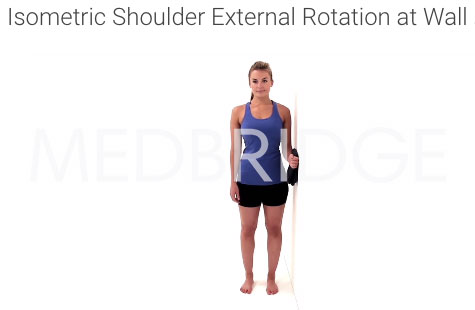
A new version of management would include early referral to PT after ACL tear with treatment for about 10 weeks. During that time, the medical team would attempt to classify the patient as a coper or non-coper. Ultimately, If the patient does need ACLR, he/she would potentially improve post-surgical outcome by completing “prehab”.
Risks
Interesting, OA rates are actually higher in subjects that had surgery than those who did not.1 There was no difference in rates of meniscus surgery between the ACLR group and the conservative care at five years.2The biggest risk in the “coper” group is opting for ACLR at a later date.
Disclaimer
Non-operative management of highly active individuals remains controversial. The science is “young” on this question. The conservative treatment findings are based on one RCT. Further replication study needs to be completed before we can confirm if a group of “copers” really exist and what complications might arise with opting out of ACLR. Admittedly, Monk et al. describe the current evidence as weak that finds no difference between conservative management and ACLR. The ability to prospectively identify individuals as true copers or non-copers is fairly poor currently.3 One could argue there is significant waste of time, resources and thus potential harm to the patient if incorrect categorization occurs.
The Future of ACL Management
We may be in the middle of a paradigm shift in which a subgroup of active people with ACL ruptures can be managed as effectively with conservative care as they can with ACL reconstruction. Consistently identifying this subgroup is proving problematic, however.3 Categorization is likely fluid and an individual can move groups after initial categorization. Depending on patient goals, a trial of conservative care for the ACL deficient may be warranted.1-4
References
Monk, A. Paul, et al. “Surgical versus conservative interventions for treating anterior cruciate ligament injuries.” The Cochrane Library (2016).
Frobell, Richard B., et al. “Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial.” Bmj 346 (2013): f232.
Moksnes, Håvard, Lynn Snyder-Mackler, and May Arna Risberg. “Individuals with an anterior cruciate ligament-deficient knee classified as noncopers may be candidates for nonsurgical rehabilitation.” journal of orthopaedic & sports physical therapy 38.10 (2008): 586-595.
Snyder-Mackler, Lynn, and May Arna Risberg. “Who needs ACL surgery? An open question.” (2011): 706-707.